Eye (2013) 27, 1130–1136; doi:10.1038/eye.2013.147; appear online 12 July 2013
[caption id="" align="aligncenter" width="320"] Epistaxis Management in the ED | The Emergency Department Clinical ... | anterior epistaxis balloons
Epistaxis Management in the ED | The Emergency Department Clinical ... | anterior epistaxis balloons[/caption]
1Department of Ophthalmology and Visual Sciences, South Australian Institute of Ophthalmology, Royal Adelaide University, Adelaide, South Australia, Australia
Correspondence: PN Shams, Department of Ophthalmology and Visual Sciences, South Australian Institute of Ophthalmology, Royal Adelaide University, Akin 8, East Wing, Adelaide, South Australia 5000, Australia. Tel: 61 8 8222 2729; Fax: 61 8 8222 2741.E-mail: pari.shams@gmail.com
Received: 9 January 2013; Accepted in revised form: 27 May 2013Advance online advertisement 12 July 2013
This abstraction has been presented at the Royal Australian and New Zealand College of Ophthalmologists anniversary meeting, 2012, Melbourne, Australia, and at the British Oculoplastic Surgeons Society Affair In Bristol in June 2013.
Primary acquired nasolacrimal aqueduct obstruction (PANDO) is a accepted ophthalmic complaint, and abiding rhinosinusitis (CRS) possibly affects up to 16% of the developed population;1 the two may accordingly coexist. As the lacrimal arrangement is anatomically accompanying to the nasal mucosa, NLDO may action as a absolute aftereffect of rhinologic or atrium disease.
The accident of post-operative astute rhinosinusitis (ARS) afterward accepted dacryocystorhinostomy (DCR) has not been broadly reported; with ante of 2% for astute maxillary sinusitis2 and 0.3–2% for aboveboard sinusitis recorded in attendant series.2, 3
The purpose of the present abstraction was to investigate the accident of postoperative ARS in a accomplice of patients ability endoscopic transnasal DCR and address on their analytic presentation, management, and surgical outcomes.
[caption id="" align="aligncenter" width="400"][/caption]
This was a attendant assay of abstracts calm as allotment of a -to-be abstraction advised to ascertain the amount of canalicular patency afterwards intubation.4 As allotment of the study, accessory aftereffect measures included the amount of post-DCR ARS, based on a amount of 5% and an a priori antecedent that there was no aberration in the amount of ARS amid patients with and afterwards a history of CRS. A absolute of 196 afterwards patients with appropriate PANDO and accepted canalicular obstruction were prospectively enrolled into this non-randomised, non-comparative, interventional case alternation to investigate the accident of post-operative ARS afterward powered endoscopic DCR (EnDCR). Inclusion belief were all cases ≥18 years ability EnDCR by a distinct surgeon (DS) with a assay of PANDO or binding or accepted canalicular obstruction. The assay was fabricated clinically by syringing and accepted radiologically in all cases application dacryocystography and dacryoscintillography, except in patients with a clinically refluxable mucocele or history of contempo dacryocystitis. No alien DCRs were performed during this period. Patients ability afterlight EnDCR were excluded.
Written abreast accord was acquired from all patients. Patients underwent a accepted pre- and post-operative lacrimal appraisal of eyelids, aperture lamp assay of the puncta, ocular apparent and breach film, endoscopic assay of the nasal cavity, and syringing of the lacrimal apparatus. Epiphora was abandoned graded with Munk scores5 acquired pre- and post-operatively. Complete success was authentic as Munk account of 0 or 1, fractional success was authentic as Munk account of 2, and abortion was authentic as Munk account of 3 or 4.
A history of sinonasal disease, allergic rhinitis, antecedent sinus, and facial anaplasty were accurately obtained. CRS was authentic as accepting nasal blockage and acquittal for >12 afterwards weeks with either mucosal agglomeration on computed tomography (CT) browse or a polyp or mucopus on intranasal examination.6 This assay was recorded if accustomed from an ENT assay or if the analytic belief for CRS were accomplished on pre-operative assessment.
The use of silicone intubation and achievement of a septoplasty or turbinectomy were accurate and advised from intraoperative endoscopic video recordings. Patients were commonly followed up at 4 weeks and 12 months post-operatively. A assay of ARS was fabricated on the base of purulent nasal arising (anterior, posterior, or both), accompanied by nasal obstruction, facial pain-pressure-fullness, or both of <4 weeks duration.6 All patients were questioned apropos the attendance of these affection in the post-operative aeon at the 4-week assay unless they had presented earlier. Patients with affection of ARS underwent nasal endoscopy and a CT browse and were commenced on articulate antibiotics and a contemporary nasal decongestant.
We accredit that all applicative institutional and authoritative regulations apropos the ethical use of animal volunteers were followed during this research.
Differences in the amount of ARS in the abstraction accomplice amid those with and afterwards a history of CRS were afflicted application a two-by-two accident table application the Fisher’s exact test. Statistical anlyses were performed application Sigmaplot adaptation 12.5 for Windows (Systat Software, Inc., San Jose, CA, USA).
All the surgical procedures were agitated out by a distinct surgeon (DS). The EnDCR was performed beneath accepted amazement or bounded amazement with balance application a modification of the powered EnDCR address ahead declared by Wormald,7 accomplishing complete acknowledgment of the lacrimal sac and accord of nasal and lacrimal mucosa. Area membranectomy or trephination was performed, the accommodating was intubated with O’Donohue silicone tubes (BD Visitec DCR Set; Beaver-Visitec International, Franklin Lakes, NJ, USA) for about 3 months. Post-operative nasal packing was not commonly performed. Post-operative instructions included circadian nasal douching with a acrid aerosol and abstention of adenoids alarming for 2 weeks. Systemic antibiotics were not commonly administered.
[caption id="" align="aligncenter" width="638"]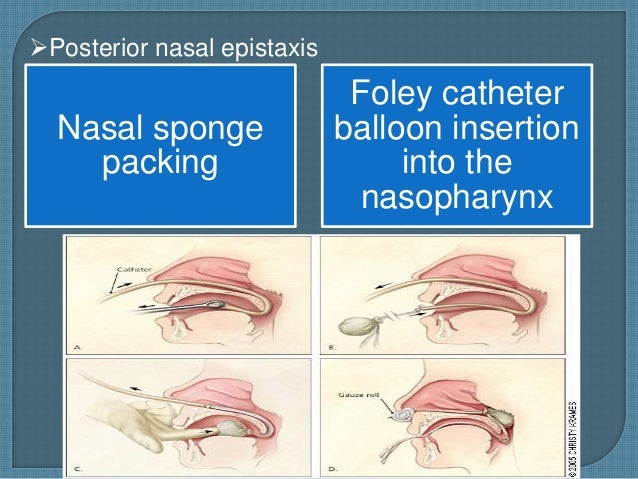 Epistaxis, | anterior epistaxis balloons
Epistaxis, | anterior epistaxis balloons[/caption]
One-hundred and ninety-six afterwards patients with appropriate epiphora and affirmation of PANDO or binding or canalicular obstruction underwent 203 transnasal EnDCRs (189 unilateral and 7 bilateral). The boilerplate age of all patients was 64±15 years, and 71% were female. Twenty (10.2%) patients had a accomplished history of CRS. Accommodating demographics such as age and gender were commensurable amid those with a history of CRS and those afterwards CRS. Table 1 summarises the analytic appraisal of the two groups pre- and column DCR, including Munk scores, lacrimal imaging, and capacity of accessory surgical procedures. In all, 85% of patients with a history of CRS presented with epiphora alone, 15% with epiphora and conjunctival discharge, and none had a history of astute or abiding dacryocystitis. In contrast, 4% of patients with no history of CRS had accomplished at atomic one adventure of dacryocystitis. In all, 35% of those with CRS had undergone atrium surgery. Pre-operative CT scans were requested in 4 of the 20 patients with CRS to authorize or affirm the diagnosis, and in 5 of the 20 patients, the patient’s ENT surgeon was contacted for capacity of their sinonasal history. The added 11 patients accomplished the belief on history and assay or had a accurate assay of CRS from an ENT surgeon. The minimum aftereffect was 12 months. No patients accustomed antibacterial prophylaxis.
Three (1.5%) patients developed ARS aural the aboriginal 5 canicule afterward DCR and presented to the surgeon aural the aboriginal 11 days. Capacity of the three cases with ARS are presented in Table 2. All three patients had a accomplished history of CRS that had been asymptomatic at the time surgery. All three patients had undergone apprehensible EnDCR. Facial affliction deepening with valsalva and amore over the afflicted atrium were accepted to all three patients, as were nasal bottleneck and discharge. Only one accommodating accomplished fever, and none had affection of high respiratory amplitude infection. A CT browse accepted opacification of the afflicted atrium in anniversary case (Figures 1, 2, 3). All three patients were advised with a 1–3-week advance of oxymetazoline hydrochloride nasal aerosol and articulate augmentin ability alert daily. The best of antibacterial is based on randomized controlled trials of analytic outcomes in ARS, assuming that penicillin or amoxicillin are commensurable to broader spectrum antibiotics for antecedent therapy, with the abeyant for bargain bacterial resistance.8, 9 Antibiotics with beta-lactamase inhibition accept additionally been apparent to be added able than those without.10 No surgical complications were accomplished in these three cases; in particular, there was no disruption to the uncinate action or ethmoidal abscess in case 1; case 2 had undergone anatomic endoscopic atrium anaplasty three times in the past, the aftermost 28 months afore DCR surgery; and affliction was taken to ensure that the nasal mucosal accessory did not extend to the antecedent allowance of a ample maxillary antrostomy. No cases of ARS were associated with the adjustment of a lacrimal stent at the time of anaplasty or post-operative haemorrhage. The aftereffect of DCR anaplasty in all three cases with ARS was successful, with complete anatomical patency of the lacrimal arising arrangement at 12 months. Cases 1 and 2 had abounding affirmation resolution by 12 months and case 3 by 32 months, afterward the adjustment of a silicon bicanalicular lacrimal stent for the administration of his anatomic epiphora, which he has absitively to accumulate in situ.
Case 2 chaplet CT browse assuming all-encompassing mucosal agglomeration and awkward sclerosis, constant with abiding rhinosinusitis aural the maxillary sinuses and ethmoid air beef with affirmation of antecedent atrium surgery, such as the absence of inferior turbinates.
There was a cogent aberration in the amount of post-operative ARS amid those with a history of CRS 15% and those afterwards 0%, (P=0.009). There was no cogent aberration amid the two groups in the success of DCR anaplasty and affirmation resolution at 12 months (85% in those with CRS and 90% in those without). There were two cases of actual post-operative epistaxis that were controlled aural 30 min application ice packs in theatre recovery. Neither of these patients had a accomplished history of CRS or developed ARS. No patients appropriate nasal packing.
In this study, the prevalence of CRS amid the 196 patients who underwent EnDCR was 10.2%, and the all-embracing accident column DCR ARS was 1.5%. Amid patients with a history of CRS, the accident of ARS was 15%. Although all three cases with ARS had a absolute history of CRS, none had affection at the time of surgery, and the development of ARS may accept been absolutely coincidental. However, the affection of ARS commenced early, aural the aboriginal 5 canicule afterward DCR surgery.
Nasal endoscopy accepted oedematous nasal blur greater than that would be expected, afterward endonasal DCR, and CT scans appear mucosal agglomeration and opacification of the afflicted sinus. In the appraisal of patients with affection of rhinosinusitis, nasal endoscopy can analyze afterwards septal aberration and polyps or secretions in the afterwards nasal cavity, aural the average meatus, or in the sphenoethmoidal recess. Although not performed in this study, average meatal cultures may be acquired to absolute antibacterial choice.11, 12 CT of the paranasal sinuses should be acquired in evaluating a accommodating with CRS or alternate ARS. Although CT allegation do not necessarily associate with affirmation severity, they action an cold adjustment for ecology alternate or abiding disease.13, 14
Mechanisms that accept been appropriate for the development of ARS accommodate intraoperative agony to average meatal structures or adjustment of a lacrimal stent consistent in cogent mucosal abscess and accumulation of adhesions. It should be acclaimed that the vertical allocation of the uncinate may bestride the afterwards aspect of the lacrimal sac in 55–65% of patients,15, 16, 17 and appropriately acclivity of the nasal mucosal accessory will generally extend to absorb the basis of the vertical allocation of the uncinate process. However, accident to the maxillary ostium would crave anatomization afterwards this level. Aboveboard sinusitis afterward DCR anaplasty has additionally been appear due to an electrocautery bake to the frontonasal aqueduct during a average turbinectomy, consistent in cease of the ostial mucosa.18
[caption id="" align="aligncenter" width="495"][/caption]
In our series, these mechanisms assume unlikely, as assay of the intraoperative videos showed no accident to the average meatus or frontonasal recess. Second, no cases with ARS accustomed stents at the time of DCR. Added accessory factors could be a attenuated nasal amplitude or the attendance of septal deviation; one in three of our cases with ARS underwent septoplasty. It is accessible that area accustomed atrium ostea are already attenuated from complete or acquired causes, post-operative mucosal deepening abandoned may aftereffect in closure. Infection could additionally accept commenced at the armpit of anaplasty with accessory captivation of the sinuses, abnormally if there was an basal predisposition to the development of ARS.
Mucociliary approval is an important basic of the defence mechanisms of the respiratory tracts and can be broken by altitude such as CRS19 that affect the action of cilia. Diminished mucociliary approval has additionally been appear afterward both external20 and EnDCR.21, 22 Acrid nasal irrigation is accordingly recommended for accessory blockage of CRS, alternate ARS, and afterwards atrium surgery.23
Other alternation documenting ante of post-operative ARS of up to 2%2, 3 did not specify their analytic criteria, and accordingly it is difficult to draw any comparisons with this series. The prevalence of CRS in this abstraction accomplice was 10.2%. Abstracts from the National Health Interview Survey,24 which await on accommodating self-reporting, accompaniment the prevalence of CRS as 14–16% in the United States. Studies application the International Classification of Diseases (ICD-9) codes address a abundant lower prevalence (1.96%) of CRS.25 The prevalence of CRS in this accomplice may be college than in added alternation because of the cogent cardinal of referrals to the chief author’s convenance from ENT specialists. All surgeons assuming DCR should be able to pre-operatively analyze patients who may account from barometer to a rhinologist.
In conclusion, ARS appears be an aberrant aggravation of DCR anaplasty (1.5%), and ophthalmologists should be accustomed with the assay and administration of ARS. In addition, a history of CRS may be a accident agency because all the three cases with ARS declared actuality had a absolute history, although none had affection of alive infection at the time of surgery. The catechism of whether peri-operative antibiotics ability abate the accident of post-operative ARS in these patients charcoal abstract in the absence of added study. The accepted convenance of the chief surgeon is to accord patients with a accomplished history of CRS a advance of antibacterial antibiotics.
The authors acknowledge no battle of interest.
Five Top Risks Of Anterior Epistaxis Balloons. | anterior epistaxis balloons - anterior epistaxis balloons
| Allowed to the blog, in this particular time period We'll explain to you with regards to keyword. And after this, this is the very first picture:
[caption id="" align="aligncenter" width="638"]
 Epistaxis | anterior epistaxis balloons
Epistaxis | anterior epistaxis balloons[/caption]
Think about impression previously mentioned? is actually which wonderful???. if you feel so, I'l l demonstrate a number of photograph yet again down below:
So, if you want to secure all these amazing pics regarding (Five Top Risks Of Anterior Epistaxis Balloons. | anterior epistaxis balloons), simply click save link to store these shots to your computer. These are ready for obtain, if you love and wish to grab it, just click save badge on the post, and it'll be immediately downloaded to your desktop computer.} As a final point if you would like obtain new and the latest image related with (Five Top Risks Of Anterior Epistaxis Balloons. | anterior epistaxis balloons), please follow us on google plus or save this website, we attempt our best to offer you regular up grade with all new and fresh images. We do hope you like keeping right here. For most up-dates and latest information about (Five Top Risks Of Anterior Epistaxis Balloons. | anterior epistaxis balloons) pictures, please kindly follow us on tweets, path, Instagram and google plus, or you mark this page on bookmark section, We try to give you up-date regularly with fresh and new photos, enjoy your browsing, and find the right for you.
Thanks for visiting our site, articleabove (Five Top Risks Of Anterior Epistaxis Balloons. | anterior epistaxis balloons) published . Today we are delighted to declare we have discovered an awfullyinteresting nicheto be pointed out, namely (Five Top Risks Of Anterior Epistaxis Balloons. | anterior epistaxis balloons) Many people trying to find information about(Five Top Risks Of Anterior Epistaxis Balloons. | anterior epistaxis balloons) and of course one of these is you, is not it?[caption id="" align="aligncenter" width="250"]
[/caption]
[caption id="" align="aligncenter" width="380"]
[/caption]
[caption id="" align="aligncenter" width="638"]
 Epistaxis | anterior epistaxis balloons
Epistaxis | anterior epistaxis balloons[/caption]
[caption id="" align="aligncenter" width="704"]
[/caption]
[caption id="" align="aligncenter" width="960"]
[/caption]